The shoulder is a ball-and-socket type of joint and is anatomically referred to as the gleno-humeral joint, describing the two bony structures involved. The socket is the glenoid cavity, a cup-shaped piece of bone that juts out from a corner of the shoulder blade (scapula). The rim of the glenoid is formed by cartilage called the labrum. The ball that fits into the socket is the head (upper part) of the humerus (arm bone). The upper (superior) part of the labrum anchors one of the two tendons of the biceps muscle . The feature that makes SLAP possible is the way the upper biceps tendon hooks over the head of the humerus. If the arm is forcefully bent inward and twists at the shoulder, the humeral head acts as a lever and tears the biceps tendon and labrum cartilage from the glenoid bone in a front-to-back (anterior-posterior) direction. And that is how the name SLAP is derived - Superior Labrum Anterior-Posterior or, in plain English, Upper Rim Front-Back. 
SLAP Lesion - pull-off of the Labrum (pink) from the Glenoid.
SLAP lesion seen from the side, with the Humeral Head removed. The front of the shoulder is on the left.
Animated Mechanism of SLAP tear.
Animated Mechanism of SLAP tear.
Causes and Risk Factors
Risk Factors: Overhead and contact sports pose a greater risk of labral tears (SLAP lesions).Often an initial forceful movement of the labrum attached to the biceps tendon to be torn away from the bone (glenoid). This is often associated with a Dislocation of the joint. If the initial condition does not heal properly, pain will result and worsen over time. Possible Causes: Injury and Trauma Treatment Painkillers and anti-inflammatories – help control the pain Surgery – SLAP lesions are usually repaired by keyhole surgery (arthroscopically) through 2 or 3 small incisions. Some SLAP lesions can be simply debrided and cleaned, whilst most need repairing depending on the severity of the lesion. The associated lesions are also treated such as labrum and ligament lesions with Instability. Prevention Strong shoulder muscles remain the best defence against shoulder injuries. Exercises that build up these muscles around the shoulder should be done. Adequate warm-up before activity and avoidance of high-contact sports will help prevent of an instability-causing injury. Shoulder SLAP Repair This is carried out under a general anaesthetic. It involves repairing the torn labrum arthroscopically (keyhole). The doctors will discuss your individual surgery with you before the operation. The operation involves reattachment of the torn labrum (see picture below). This usually done using sutures and small bone anchors.
Normal Biceps and Superior Labrum
 SLAP Lesion  SLAP repaired with suture (blue) attached to an anchor in the glenoid bone.
For Interactive Animations see Interactive Surgery - go to [Shoulder] then [Instability & Labrum Problems] and [SLAP Lesion Repair].
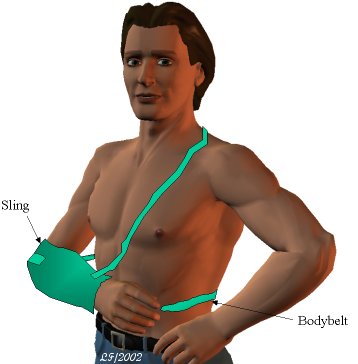
You must not eat or drink anything after midnight the day before your surgery. When you wake up following the procedure you will be wearing a sling with a body belt (see picture). The sling should be worn under the clothes for 3 weeks. The body belt can be removed at 3 weeks and you can begin wearing the sling outside your clothing, but the remaining sling is to be continued for a further 3 weeks. For more details on Living with a Shoulder Sling CLICK HERE
You will probably be in hospital overnight after your operation. A physiotherapist will see you in hospital to teach you the appropriate exercises. You may also see an occupational therapist to give you advice regarding the use of your arm.
 PAIN
A nerve block is usually used during the surgery. This means that immediately after the operation the shoulder and arm often feel completely numb. This may last for a few hours. After this the shoulder may well be sore and you will be given painkillers to help this whilst in hospital. These can be continued after you are discharged home. Ice packs may also help reduce pain. Wrap crushed ice or frozen peas in a damp, cold cloth and place on the shoulder for up to 15 minutes. Ensuring you cover the wound site with a piece of cling film to keep the area dry.
THE WOUND
This keyhole operation is usually done through two or three 5mm puncture wounds. There will be no stitches only small sticking plaster strips over the wounds. These should be kept dry until healed. This usually takes 5 to 7 days.
SLEEPING
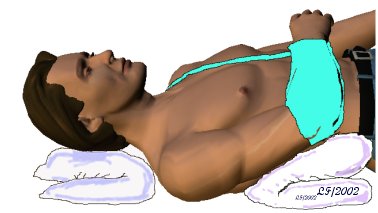
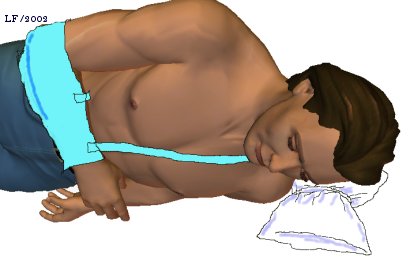
For the first six weeks your sling must be worn in bed. Sleeping can be uncomfortable if you try and lie on the operated arm. We recommend that you lie on your back or on the opposite side, as you prefer. Ordinary pillows can be used to give you comfort and support. If you are lying on your side one pillow slightly folded under your neck gives enough support for most people. A pillow folded in half supports the arm in front and a pillow tucked along your back helps to prevent you rolling onto the operated shoulder during the night. If you are lying on your back, tie a pillow tightly in the middle (a "butterfly pillow") or use a folded pillow to support your neck. Place a folded pillow under the elbow of the operated arm to support that.
  An appointment will be made for you to see a physiotherapist after your discharge and you will be seen by the Shoulder Team 3 weeks post-operatively. DAILY ACTIVITIESFor the first six weeks all activities of daily living for example feeding, dressing, cooking etc must be carried out using your un-operated arm. If appropriate an occupational therapist will be available to give you advice on how to do this.LEISURE ACTIVITIESYour physiotherapist and surgeon will advise you when it is safe to resume your leisure activities. This will vary according to your sport and level, as well as the period required to retrain your shoulder muscles with physiotherapy.Below is a rough guide:
DRIVING
You will not be able to drive for a minimum of 8 weeks. Your surgeon will confirm when you may begin.
RETURNING TO WORK
This will depend upon the size of your tear and your occupation. You will need to discuss this with a member of the Shoulder Team
19/02/2004
|
воскресенье, 24 мая 2015 г.
SLAP Lesions
Подписаться на:
Комментарии к сообщению (Atom)
Комментариев нет:
Отправить комментарий